
Homeostasis and glucose regulation

Homeostasis:
Definition of homeostasis?
The term homeostasis (from a Greek word meaning staying the same) is used to mean maintenance of static or constant conditions in the internal environment of the body. It describes all mechanisms by which a constant environment is maintained in the body.
Why homeostasis is necessary?
It is so because cells can only function properly within narrow ranges of conditions. The body has to keep the proper concentration of oxygen, glucose, osmotic pressure, temperature, pH, the different electrolytes such as potassium and sodium and other nutrients in the body to allow the cells to function efficiently.
Mechanism of homeostasis
- Negative Feedback: is a mechanism whereby deviation from a set norm causes a corrective mechanism to restores the norm. For example, an increase in the concentration of glucose in blood initiates mechanism that brings the concentration back to normal.
An efficient negative feedback mechanism is the one that detects small changes from the norm and responds fast to prevents big fluctuations from the set point
For the corrective mechanism to work there must be
- Reference point- The set level at which the system operates
- Detector – signals the extent of any deviation from the reference point.
- The controller (brain)- coordinates the information from various detectors and sends out instructions which will correct the deviation.
- Effector – brings about the necessary changes needed to return the system to the reference point.
- Feedback loop-informs the detector about the necessary changes in the system as a result of action taken by the effector.
2. Positive feedback:
is a mechanism whereby the deviation from the norm causes further deviation. When a person is caught up in a burning building, high temperature increases the activity of enzymes which results in further heat production. A positive feedback mechanism leads to death.
Examples of positive feedback mechanisms
- Childbirth
During labor release of oxytocin intensifies and speeds up the contraction. The increase I contraction causes more oxytocin to be released and the cycle goes on until the baby is born
2. Blood clotting
Once a vessel is damaged, platelets start to cling to injured site release chemicals that attract more platelets. The platelets continue to pile up and release chemicals until a clot is formed.
The homeostatic control of glucose.
The normal concentration of glucose in human blood is approximately 90mg per 100 cm3, and even after the heaviest carbohydrate meal rarely exceeds 150mg per 100cm3. After absorption from the gut, various things can happen to glucose in the body.
- It is broken down into carbon dioxide and water, particularly in active tissues such as the muscles.
- It may be built into glycogen and stored.
- It may be converted into fats and stored in the body’s fat depots.
- If glucose is in short supply, glycogen may be broken down into glucose.
The concentration of glucose in the blood and tissue fluids at any moment is determined by the relative extent to which these different processes occur in the body.
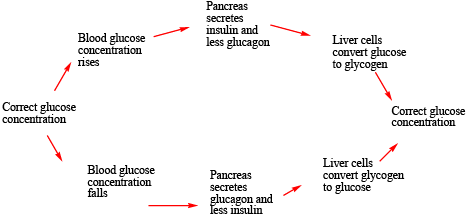
For example, if there is too much glucose, as after a large meal rich in carbohydrates, the liver cells convert glucose to glycogen lowering its concentration in blood. When the concentration of glucose is low in blood, the liver cells convert glycogen into glucose, thereby raising the glucose concentration in the body.
In prolonged deficiency, glucose may be formed from non-carbohydrate sources, including fat and proteins. This is called gluconeogenesis. This explains the wasting away of tissues, which occur in extreme starvation. This is because the body resorts to converting its tissue proteins into carbohydrates.
The role of the pancreas in glucose regulation.
A high concentration of glucose in the blood triggers the pancreas to secrete the hormone insulin from β-cells of islets of Langerhans. This insulin exerts its effect lowering the blood glucose level mainly by
- increasing the conversion of glucose to glycogen and fat by the liver cells.
- inhibiting the formation of glucose from glycogen and non-carbohydrate sources (gluconeogenesis).
- Increasing oxidation of glucose into carbon dioxide and water.
Low concentration of glucose in the blood triggers the pancreas to secrete the hormone glucagon from α-cells of islets of Langerhans and inhibits the secretion of insulin. This increases the concentration of glucose by
- Causing liver cells to convert glycogen and fat by the liver cells.
- Promotes gluconeogenesis or the formation of glucose from glycogen and non-carbohydrate sources
The homeostatic scheme of control of glucose in the mammalian body is shown below
Diabetes mellitus
is a disease condition caused by the inability of an individual’s pancreas to produce enough insulin. It is characterized by an increased in the blood glucose concentration (hyperglycemia), and glucose appears in urine (glycosuria). The production of urine increases and the patient may suffer from intense thirst. Later symptoms include severe loss of the body mass, muscular waste, and skin lesions. If untreated the patient goes into a diabetic coma and dies.
Diabetes mellitus is controlled by appropriate doses of parenteral insulin.
For examination sample questions, download the link below
Homeostasis (principles) and regulation of glucose in blood
Please find free downloadable notes, exams and marking guides of agriculture, biology, Physics, chemistry etc. from digitalteachers.co.ug website.
Dr. Bbosa Science

This is so wonderful really you have made science easier accessible and affordable wherever IAM thanks to Science Foundation College for sponsoring such a wonderful work and Dr Bossa for content mastery and delivery
Your insights always resonate with me. Industrial & Scientific
I’m eagerly awaiting your next post! Tech News
The Top MBBS Colleges in Andhra Pradesh offer unmatched training and academic excellence.
Learn about qualifying scores for top institutions at MBBS Cutoff Of Government Medical Colleges in Punjab.
Learn how Raja Luck is evolving over time.
Catch all the latest updates and highlights of Indian Football in Bengali.
Discover flexible rental strategies with innovative Server Rental in Gurgaon that fulfill your organization needs.